The number of people in England undergoing surgery on the NHS to help them lose weight has increased ten-fold in less than a decade.
The British Medical Journal (BMJ) reports operations such as gastric banding and bypasses rose from 238 a year to more than 2,543 in 2007.
Researchers from Imperial College London said more obese patients were now aware that surgery could help them.
The Department of Health said drugs and surgery should always be a last resort.
Experts at the National Institute for health and Clinical Excellence (NICE) recommended in 2002 that people classed as “morbidly obese” should be considered for surgery if other weight-loss methods had failed.
Safer techniques
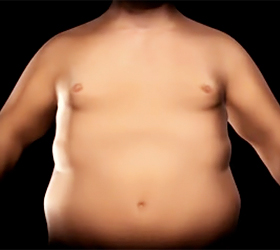
In simple terms the operations, sometimes called “bariatric surgery”, work by restricting the amount of nutrients that can be digested and absorbed by the intestine.
Gastric banding involves reducing the size of the stomach with a band fitted around it, while a gastric bypass reroutes food to a small stomach pouch created by surgeons. A third, less frequently used procedure, removes a portion of the stomach.
The Imperial researchers, led by Dr Omar Faiz, found that three-quarters of the operations were carried out using “keyhole” techniques, which avoid the need for a large surgical incision, and that there was no evidence of any safety problems despite the swift increase in the number of operations across the NHS.
However, they did not look into whether the operations actually helped the patients lose weight.
Between April 2000 and March 2008, when the study data ended, there were 6,953 operations carried out by the NHS.
In 2000, there were only 238, while in 2007, there were 2,543.
The research team said: “Bariatric surgery has increased exponentially in England in recent years.
“In conjunction with the growing level of obesity, as patients become more aware of surgery as a viable treatment option, demand for surgery among morbidly obese patients increases.”
They said that primary care trusts, who currently decide which treatments to fund in local areas, should be encouraged to pay for obesity surgery.
Paul Aylin of Imperial College, who wrote the BMJ report, said evidence was growing that the procedures were effective in some obese patients.
“Very extreme obesity is associated with all sorts of other illnesses like diabetes, high blood pressure, and heart disease,” he told Today.
“Evidence is emerging now that these sorts of operations can reduce those other illnesses.”
Peter Sedman, a bariatric surgeon and spokesman for the Royal College of Surgeons said: “We are beginning to catch up with a backlog that has been building for decades, and we are only now beginning to catch up with the US and other European countries in providing this care.
“The number of morbidly obese patients in the UK is increasing rapidly and we need to continue to put even more resources in to what is proven to be a successful and cost-effective method of treatment. The burden on the NHS in years to come in obesity-related illness will otherwise be overwhelming.”
Chrissie Palmer, at the British Obesity Surgery Patients Association, which helps provide information and support to patients considering or undergoing weight-loss surgery, said the rise in operations was welcome.
However, she said: “There are still places in the UK where weight-loss surgery is not taking place on the NHS, despite the advice from NICE.”
She added that there was still some stigma wrongly attached to it despite the enormous lifestyle changes required by patients both before and after.
“I don’t think people understand what a large commitment is involved – people have to change their behaviour for life, although once they start feeling the benefits, it becomes easier.”
Health minister Paul Burstow said people should be encouraged to eat more fruit and vegetables, reduce the amount of fatty foods they eat and be more active.
“Our ambition is to encourage healthier lifestyles and reduce the need for this type of treatment.”
And a Department of Health spokesman added: “Independent guidance on obesity from NICE recommends that drugs and surgery should always be a last resort – a better diet and more exercise should be tried first.
“It is up to individual trusts to commission a range of services to meet their local community’s needs.”
Delia Stearnes was 19-and-a-half stone (124kg) when she paid to have her own gastric band fitted in January in a “spur of the moment” decision.
The 58-year-old told BBC Radio 4’s Today programme shifting weight is not just as simple as eating less and healthier.
“I had lost three-and-a-half stone with Slimming World before, so I’d had a head start, but the thing is with weight loss, you can lose the weight but you just put it back on again eventually,” she said.
“When you start dieting, your body thinks starvation mode, and shuts everything down and then when you start eating again – even if you’re not binge-eating – it puts the weight back on.
“I personally probably don’t need many calories at all to maintain my weight, whereas some people need a lot of calories to maintain their weight.
“I think there’s more to it. I’ve had guilt heaped on me all my life really, so I think people are beginning to realise there may be a bit more to it.”
How gastric bands work
- Gastric band fitted around the upper end of the stomach
- This restricts flow of food into the lower stomach
- Band can be adjusted via the access port